Chris is the Radiotherapy Equipment Manager at Leeds Teaching Hospitals NHS Trust. In his blog he talks about the role of clinical technologists and what led him down this particular career path. He shares some of his accomplishments so far – including a rather nice mission in the Med!
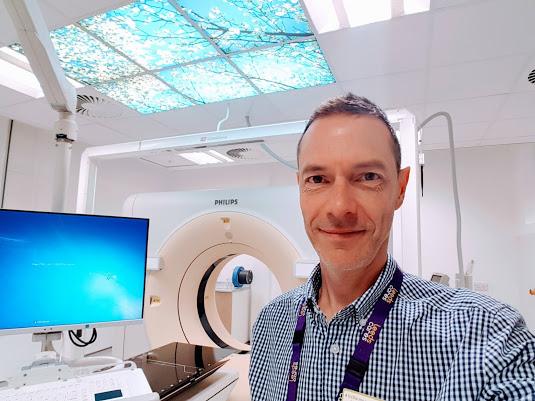
I’m a clinical technologist in the radiotherapy department at Leeds. I’m part of the clinical team who manages the implementation and maintenance of the complex radiotherapy technology that delivers the clinical radiotherapy service for our patients.
So, what led me to this career? Well, as a teenager, I was an electronics hobbyist with a passion for wanting to understand ‘how stuff works.’ I started my NHS career at age 17 as a student technician, initially repairing simple patient monitoring equipment under supervision. After a few weeks, I saw the radiotherapy technology environment. It seemed much more exciting, so I moved into the radiotherapy team without looking back. I spent several years gaining qualifications, maintaining radiotherapy equipment and fostering relationships with my radiographer and scientist colleagues to really understand clinical processes and workflows, before developing the scope of my role.
I specified and project-managed the new building and refurbishment schemes of our radiotherapy facilities. I was very lucky to be offered a key role in the design and commissioning of our new oncology centre, which opened in 2008. One of the more unusual projects I’ve been involved in was to project-manage the commissioning of a new radiotherapy centre on a small (and very sunny) Mediterranean island.

As well as the usual clinical and technology challenges, we also had logistical ones, which included getting our specialised equipment overseas, researching accommodation, communications, flights, car hire and even local health services for our team. I was amazed at the innovation brought into the project by our staff, including our brilliant data communications team. They set up video conferencing and allowed us to pick up the phone 1400 miles away and dial an internal extension number as if we were sat at our desks back in Leeds. I also developed a bit of a reputation as a local restaurant and tour guide: evidence-based, of course!
The equipment we manage at Leeds includes linear accelerators (linacs), CT-simulators (specialised CT scanners for radiotherapy planning), patient immobilisation devices, brachytherapy and equipment used for stereotactic radiotherapy. These are what I call the ‘visible’ technologies. We also implement and manage clinical computing technology such as treatment planning systems, oncology patient information systems, image processing, quality assurance and many other systems providing critical radiotherapy software applications and clinical data.
We see our roles as clinical technologists in a progressive healthcare environment as having three key objectives: first, to keep the technology safe and reliable. Second, to make the technology work for us as efficiently and effectively as possible by using the best and most up-to-date technology management methods. Third, and perhaps most rewarding, to develop and progress the use of the technology to advance clinical practice.
Our radiotherapy service is underpinned by an expert team of multidisciplinary professionals. Clinical technologists work together with therapeutic radiographers, medical physicists, clinical oncologists and equipment manufacturers to develop new processes and introduce new technology for the benefit of our patients. To make projects work for us, we all get together at project meetings and tap into each other’s experience and expertise. We discuss the challenge, how it will make things better and how we’re going to achieve it. This could be by making the treatment more accurate, more comfortable, more efficient and wherever possible, more effective. This may mean we have to devise a plan to use our existing equipment in a slightly different way, or even design a completely new medical device. Our roles dictate that we have a good understanding of legislation such as the Medical Device Regulations and best practice issued by organisations such as the Medical and Healthcare Regulatory Agency (MHRA). If we can’t buy equipment that can solve the clinical challenge, then we can often design and make it, utilising new prototyping and production techniques such as 3D printing technology.

One theme we’re focussing on currently are technology solutions to display and collect clinical information in the right place and at the right time. With this objective in mind, we developed a system that allows our radiographers to display patient data, acquire ID photographs and enter treatment setup instructions during CT-simulation, without having to move from the patient’s side.
What about the future? The next big thing to arrive in radiotherapy departments is magnetic resonance imaging. It’s going to be a real game-changer and I’m excited to wear my clinical-technologist badge and project-manager hat for our MRI-simulator when it lands in Leeds very soon!
