Richard Simcock, Consultant Clinical Oncologist, specialising in Breast and Head and Neck Cancer at Brighton and Sussex University Hospitals NHS Trust.

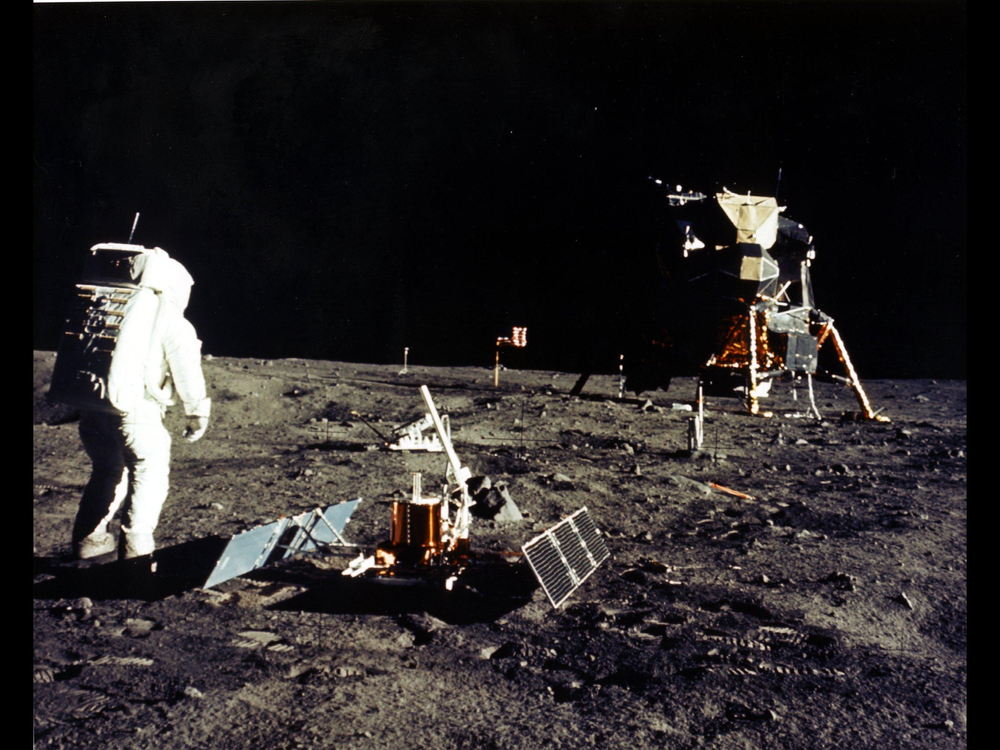
Fifty years ago, we landed on the moon. Space exploration continues, but those iconic images of Neil Armstrong on the lunar landscape are still symbolic of humanity’s technological progress.
Another technology has important origins in 1969. This is when the World Health Organization Committee of Investigators for Evaluation of Methods of Diagnosis and Treatment of Breast Cancer approved a trial led by a young Italian researcher, Umberto Veronesi. Veronesi believed the standard ‘Halsted Mastectomy’ was an unnecessarily mutilating operation for small breast tumours and set out to prove that radiation and a smaller operation (a quadrantectomy) would be as effective. He enrolled his first patient in Milan, and subsequent analysis in 1977, 1981 and most recently in 2002 showed equivalent survival with both treatment approaches. Veronesi identified a fact that is still true today: surgery to remove a tumour and leave the breast intact followed by radiotherapy to the whole breast is as effective as a mastectomy.
Tens of thousands of women worldwide have since benefitted from radiotherapy and safely kept their breasts after a diagnosis of cancer. This achievement might have been enough in itself – our cancer version of the lunar landing – but there is always more to learn. To quote the comedian, Dara Ó Briain: ‘If science knew everything, it would just stop’ (YouTube video link with auto-playing sound). Radiotherapy research doesn’t stop: it relentlessly refines.
Since 1969, every aspect of breast radiotherapy has improved. It continues to evolve, making therapy safer and more accurate, with shorter treatment durations and fewer side effects.
Radiotherapy is delivered over a course of daily treatments (fractions), usually Monday to Friday. In Veronesi’s work, the standard was to deliver treatment in 25 fractions (five weeks). Fractionation can be changed successfully, but it needs to be done carefully. Imagine a cake: it is possible to cut the same cake into a just a few large slices or cut it into several small slices. The important question is whether the effect is the same. A cake eaten in just one or two large slices may make you sick, but one small crumb every day for several months will hardly impact at all. The UK START trial was globally practice-changing, demonstrating that breast radiotherapy treatment could be safely and effectively given in 15 fractions (over three weeks), saving each patient ten round trips to the hospital and all the associated inconvenience. Further research is now investigating whether just five treatments are as safe and effective for some women.
The smallest possible number of radiation sessions is of course none, and it is recognised that radiotherapy may be unnecessary for many women who are cleared of their disease by surgery. UK radiotherapy research has identified groups of older women who can avoid the treatment altogether. Using modern biotechnology, ongoing research is now looking for genetic patterns in tumours, which will allow further tailoring of the radiotherapy prescription.
Analysis of older studies shows that breast radiotherapy given in the past inadvertently caused harm by exposing the nearby heart to unnecessary radiation. Newer treatments avoid this risk with techniques that track the patients breathing or only irradiate when the heart is out of the way. These technologies make radiotherapy safer than ever before. Accuracy in breast radiotherapy is usually assisted by small tattoos on the patient, which are matched with a laser position. These tiny ink marks can be an unwelcome reminder of cancer for some, and so innovations including UV tattoo ink and camera-position tracking are being developed and implemented to make tattoos redundant.
Radiotherapy is an excellent targeted treatment and there has been considerable work in refining targeting. For instance, in high-risk disease, research has shown life-saving advantages such as including the lymph glands behind the breast bone in the radiation treatment region. Historically, these glands were difficult to treat without excessive doses of radiation to the lungs and heart, but hardware and software developments now make this routinely possible. At the low-risk end of the spectrum, UK research has shown that treatment to only part of the breast is safe: made possible by using careful targeting technologies.
Veronesi never stopped exploring radiotherapy advances. At the age of 87, he published new research on treating the breast in the smallest and shortest method possible of all: a single radiation dose given during surgery from inside the breast.
Fifty years after Apollo 11, entrepreneurs have dubious ambitions for space tourism for the lucky few who can afford it. In the same period, breast radiotherapy has advanced to represent the best of technology, but here on earth and for everybody.