Our chair and founder, Professor Pat Price, has co-authored a powerful new blueprint to tackle the UK’s cancer crisis.
The Policy Review will be launched in Parliament later today and published in The Lancet Oncology.
It could not come at a better time.
The new Secretary of State for Health and Social Care was announced on Monday: the fifth person to hold this post in just over two years. Radiotherapy UK sees this review as a huge opportunity for Victoria Atkins MP to take charge and show some serious ambition for cancer patient outcomes.

Response to poor patient outcomes and survival rates
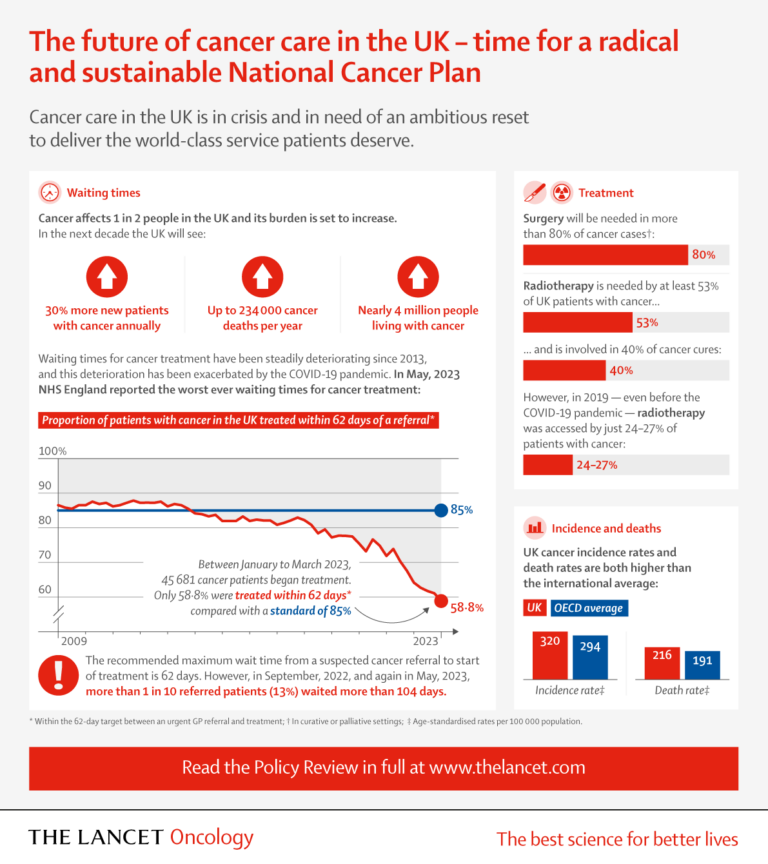
The review has been written by leading cancer expects in response to consistently poor patient outcomes and survival rates. Cancer services have been in decline since 2013, and there has been a significant failure to recover from the effects of the pandemic. With up to 2,000 extra cancer cases a week expected by 2040, action is urgently needed to stop us sleep-walking deeper into the crisis.
The authors hope to drive government-level adoption of the 10-point review, which clearly outlines the steps to a sustainable service ‘fit for the future.’
A lifeline for patients
Professor Pat Price said: “A cancer plan is not just a strategy, it is a lifeline for the 1 in 2 of us that will get cancer.
“Cancer patients are consistently being failed, with UK cancer survival outcomes remaining near the bottom of cancer league tables.
“We need to address the cancer workforce crisis, deliver treatments on time and stop the situation that sees us lagging behind on cancer technologies in key areas, like radiotherapy.
“The urgent need for a cancer specific control plan is clear, and it beggars belief that clinicians are finding themselves having to produce one instead of the Government.”
Radiotherapy UK would like to thank The Lancet Oncology and all co-authors of the plan.
Leading cancer doctors raise the alarm about “serious missteps” on cancer policy in new 10-point cancer plan to improve cancer care in the UK – The Lancet Oncology
The loss of a dedicated National Cancer Control Plan in England and Wales has been a “major misstep” at a time when the NHS is facing massive workforce shortages and cancer services have struggled to recover after the COVID-19 pandemic, caution leading cancer experts in a Policy Review published in The Lancet Oncology.
Previous research has shown a correlation between dedicated cancer control policies and better five-year overall survival for cancer patients. [1]
In light of this, the diverse group of senior clinical cancer specialists who authored the report call for the development of radical, yet sustainable, cancer control plans as they anticipate a need for a cancer service “fit for the future,” with up to 2,000 extra cancer cases a week expected by 2040.
The authors draw attention to the UK’s poor performance compared to other countries, stating that our approach to cancer care contradicts “international consensus”.
Citing research by the International Cancer Benchmarking Partnership, which demonstrates that the country’s approach to cancer is “not working,” and all UK nations were in the bottom half of cancer league tables.
Leading oncologist authors caution that the lack of a cancer plan is “an incomprehensible decision not in the best interests of people with cancer.” Therefore, the group of cancer experts has published their own 10-point plan as a blueprint for a new cancer strategy.
The report will be launched at an event in Parliament on 15 November 2023 and outlines a blueprint to tackle the cancer crisis. It highlights the action needed to tackle record cancer treatment waiting times, workforce shortages, and the lingering impact of the COVID-19 pandemic.
Professor Pat Price, joint senior author, leading oncologist and Visiting Professor Imperial College London said: “The dangerous reality is that cancer care in this country is fast becoming a monumental crisis and there appears to be no realistic plan.
Today we face record cancer treatment waiting times with an expected increase of 2000 extra cancer patients a week by 2040.
A cancer plan is not just a strategy, it is a lifeline for the 1 in 2 of us that will get cancer. Cancer patients are consistently being failed, with UK cancer survival outcomes remaining near the bottom of cancer league tables.
We need to address the cancer workforce crisis, deliver treatments on time and stop the situation that sees us lagging behind on cancer technologies in key areas, like radiotherapy.
The urgent need for a cancer specific control plan is clear, and it beggars belief that clinicians are finding themselves having to produce one instead of the Government.”
Professor Mark Lawler, Professor of Digital Health at Queen’s University Belfast, chair of the International Cancer Benchmarking Partnership and co-author on the paper said: “Abandoning a dedicated National Cancer Control Plan in favour of a Major Conditions Strategy is an incomprehensible decision not in the best interests of people with cancer.
Our previous research (published in Lancet Oncology) has shown conclusively that cancer policy consistency is associated with superior 5 year survival outcomes – getting rid of a dedicated cancer strategy will cost lives.
Dismantling the National Cancer Research Institute is also a big mistake, particularly as we have just shown through the Lancet Oncology European Groundshot Commission that cancer research is a necessity for delivering 21st century cancer care, not a luxury .”
Professor Richard Sullivan, joint senior author and Director of the Institute of Cancer Policy at King’s College London, said “Cancer needs to be a top political priority for the whole of the UK.
The awful statistic that 1 in 2 of us will develop cancer should be justification enough. We need care that is clinically led and truly personalised.
The failure to deliver specific and properly resourced cancer plans with a research agenda that is fit-for-purpose is also leading to widening patient inequalities, healthcare staff burnout and poor outcomes.
All the ingredients are there to address these issues. But we need political will”
[1] https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(22)00450-8/fulltext
