How are you? …
No, really … how are you?

There has been nearly a year of lockdowns, uncertainty, changes, and frustration to battle with during this pandemic.
When was the last time you took a step back from what is going on to check in with yourself?
Being professionals in a caring work environment, we often forget about ourselves and put others first. The duration of this pandemic will be taking a toll on everyone, including you, and it’s okay to admit that.
Everyone will be at different stages of how they are dealing with everything that is going on around them and we all have different challenges to deal with. Just because someone has no children to home-school does not mean they are not struggling: we all have our crosses to bear with this pandemic.
How have you adapted to a ‘new normal’ in an aspect of your life?
Perhaps we should liken it to the grieving process! We are mourning for our freedoms, struggling with the uncertainty of when we may hug family and friends, exploring how workplaces and social lives will look in the months and years to come. Remember we all grieve at different rates and will be at different points in the cycle. It is also possible to start at different points and bounce between points of the cycle.
Let’s have a look at the Kübler-Ross grief cycle model (1969):

Image available: https://www.psycom.net/depression.central.grief.html
Denial : denial and shock are part of the process of coping with grief. Do you know of people, or have you seen people who deny this whole situation with the pandemic is happening? Perhaps they have been labelled as ‘stupid’ for not following the rules. There may be some who are doing that, but let us also consider those in denial, and not berate them when they then move to anger.
Anger: most of us have likely been angry about the situation at some point over the last year, either through frustration or that feeling of loss. Anger is an important part of the healing process. This is not just how we feel, but if family members or colleagues are at different stages, all of us can feel the brunt of this anger and find it difficult to manage. Perhaps we, as healthcare professionals, need to be aware of where we ourselves are in this grieving process so we don’t negatively affect others.
Bargaining: ‘let us just follow the rules and we will get out of this quicker’. Have you heard this type of statement? Perhaps we feel desperate to get back to normal. Guilt is commonly associated with bargaining too. Am I doing enough? Colleagues who are shielding, on maternity leave or in other areas of the profession may feel the guilt of not being on the ‘front line’. The endless ‘what-if’ statements can make the guilt take over our thoughts and send us into a spiral.
Depression: we are aware of how low people are starting to feel as we are nearly a year into this pandemic. We’ve started to see more and more people around us with low moods, feeling anxious and being withdrawn. Depression is very much the ‘present’ emotion as it can hit you when you are least expecting it.
Acceptance: some of you will have accepted that this is just the way life is, others will fight it (through earlier stages) and think that life will go back to normal. We must have some hope that this will happen soon. Life does not need to stop: you can distinguish what is and isn’t in your control.
Whatever stage you are in, it is important to acknowledge your thoughts, feelings, behaviour and any physical symptoms you may have related to the pandemic.
Carlisle Healthcare has used the cognitive behaviour therapy (CBT) model to demonstrate how to work through our thoughts (why not give this a try?):
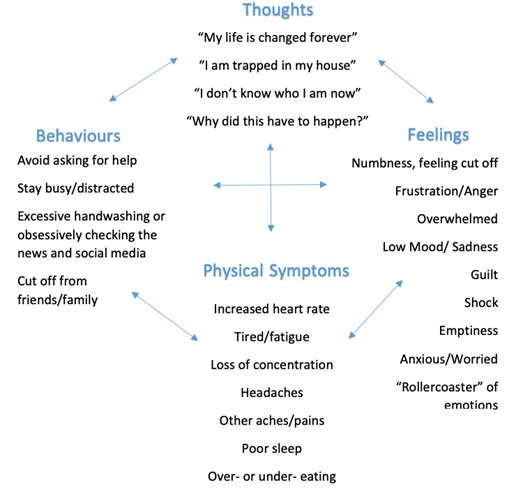
Making a change in one area will help improve another. For example, doing some gentle exercise such as going for a short walk will help improve your mood, fatigue, and possibly help you feel less trapped. This doesn’t mean you should try and change everything in one go. Take your time: do not be your own worst enemy, stay in the present and focus your energy. It is also important to consider that what works for one person doesn’t necessarily work for another. It’s important you discover what works for you and integrate it as an important part of your life.
We have had to use our energy to not only do our jobs, but to react to change at an unprecedented level. The NHS, charities and health-education workforce has been truly tested throughout this pandemic and you have certainly shown a great deal of resilience; perhaps more than you ever thought you had. This has brought some teams together and forged some unbreakable bonds, but now we must consider burnout, compassion fatigue and vicarious traumatisation.
As a profession, we have always been at risk of burnout and this has been researched and highlighted as a concern (Clarkson et al, 2019; Probst et al, 2012). Burnout is caused by excessive and prolonged stress bringing about mental, physical, and emotional exhaustion. This can lead to a diminished ability to empathise or feel compassion for others around us. Vicarious trauma affects anyone who empathetically engages with survivors of trauma, such as having their treatment delayed due to the pandemic, leading to being emotionally involved or feeling bystander guilt. Prolonged exposure to this can affect your belief systems and your values. The signs, symptoms and triggers are highlighted below. Do these resonate with you? Could you spot any of these in a colleague?
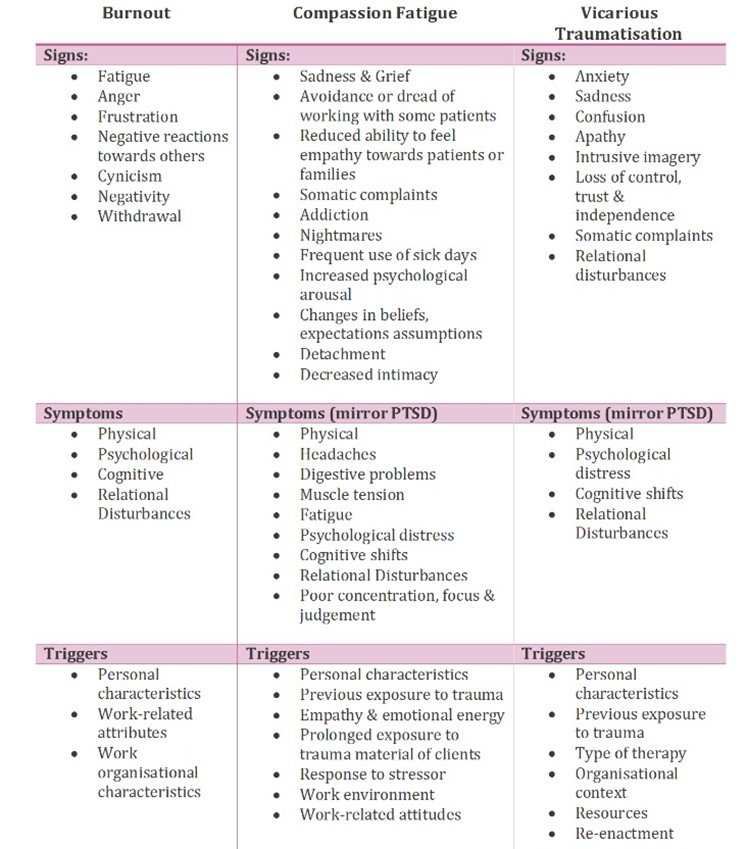
Available at: http://transitionalsupport.com.au/transitional-phase/compassion-fatigue-trauma/
Most of us feel the exhaustion now. It’s time to plan for our recovery; how our thought processes might alter to only think of that which we can control. The need for breaks provided throughout the day to be used for actual ‘breaks’, instead of trying to work through or catch up. We must now protect our emotional wellbeing and that of each other so we can continue to provide for our patients and our profession.
What can you do, not only for yourself but for others around you?
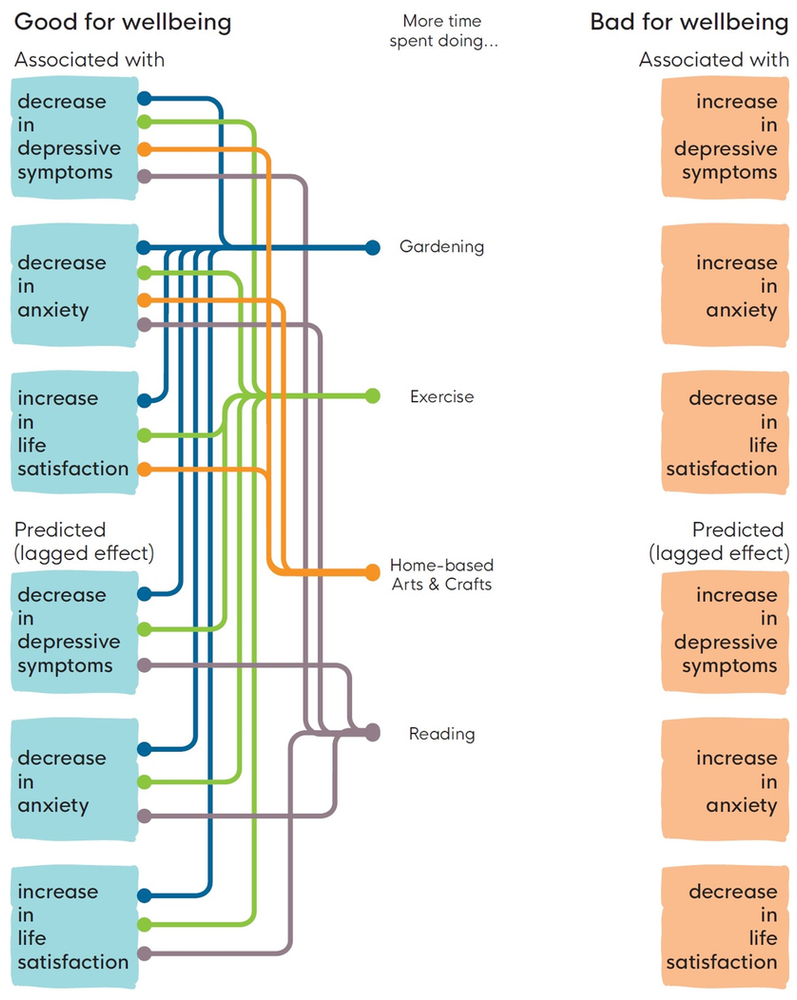
University College London (UCL) and What Works Wellbeing recently published results from their COVID-19 social study to understand the social and psychological impact of the pandemic. It is no surprise that one of their key findings showed that watching COVID-19-related news had the most negative impact on participant’s wellbeing. The figure below shows other key findings:
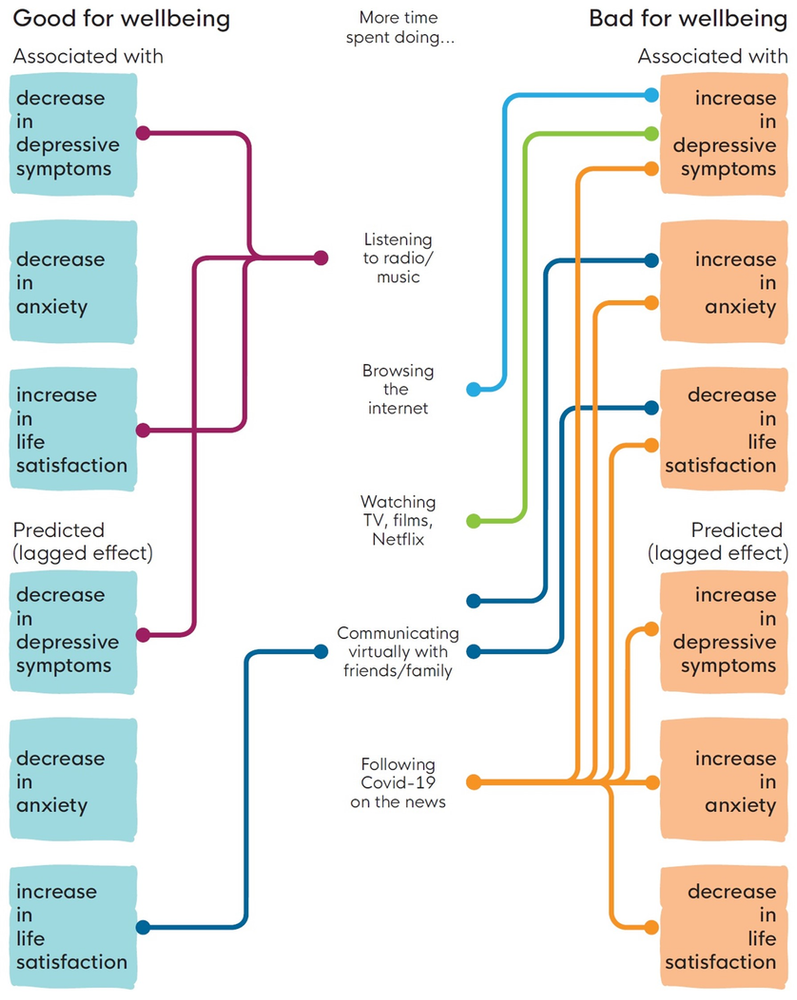
When you understand where you are in the grief cycle, you can help yourself tackle burnout early on, not only for yourself but for colleagues and friends. The COVID-19 social study summarised what participants found helped their wellbeing the most:
During the first lockdown there was a lot of wellbeing support available. At the time, you may have thought you were okay. But what about now? Has the duration of this pandemic started to take its toll? It is important to maintain wellbeing from the outset and not just when we reach rock bottom. Then, when we do need to dig deep, we have the tools readily available to improve and maintain our wellbeing and get us through tricky times. If you don’t already, make room for your wellbeing in your life; even better if there can be space in your working life as well.
As always, you are making a difference. In whatever role you have in radiotherapy, YOU make a difference to the patients, their carers, your team, and the profession. Make sure YOU make the difference to YOU as well.
Support for healthcare professionals is available via the Macmillan Cancer Support Emotional Health & Wellbeing Hub
References
1. Kubler-Ross, E., 1969. On death and dying. New York: Macmillan.
2. Psycom, 2021. Remedy Health Media. Retrieved from https://www.psycom.net/depression.central.grief.html
3. Carlise Healthcare, 2021. Retrieved from https://www.carlislehealthcare.co.uk/media/content/files/Loss%20and%20Grief%20-%20Coronavirus%20Pandemic%20PDF.pdf
4. M. Clarkson, G. Heads, D. Hodgson, H. Probst, 2019. Does the intervention of mindfulness reduce levels of burnout and compassion fatigue and increase resilience in pre-registration students? A pilot study. Radiography. 25(1); 4–9
5. H. Probst, S. Griffiths, R. Adams, C. Hill, 2012. Burnout in therapy radiographers in the UK. Br J Radiol, 85; e760–e765
6. What works centre for wellbeing, 2021. Retrieved from https://whatworkswellbeing.org/blog/what-helped-the-uk-cope-with-the-covid-19-pandemic-and-lockdowns/
7. Transitional Support, 2021. Retrieved from http://transitionalsupport.com.au/transitional-phase/compassion-fatigue-trauma/